At Create Health we offer a comprehensive 2D, 3D and 4D (active real-time motion and expression) ultrasound scanning to all pregnant women, using the latest cutting edge technology. The vast majority of ultrasound scans are done through the abdomen – although in early pregnancy and when examining the cervix and low lying placenta at any stage, the transvaginal scanning is optimal.
We also offer a comprehensive non-invasive prenatal screening by biochemical and ultrasound screening program for congenital anomalies and chromosomal abnormalities at various stages of pregnancy.
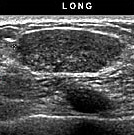
Ultrasound Diagnosis in the First Trimester
Assessment of gestational age by crown rump length. This is particularly important for any women who are unsure of their dates because of irregular periods, conception after recently stopping the pill or whilst on the pill, and conception whilst breast feeding.
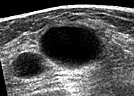
Diagnosis of pregnancy from 1 week after the first missed period. It is possible to visualize the gestational sac inside the uterus at this gestation, and confirm an ongoing pregnancy.
Diagnosis of fetal viability from 5.5 – 6 weeks. It is possible to detect heartbeat even at this early stage (1.5 – 2 weeks after the first missed period), and allows confirmation of a live fetus. Whether the pregnancy is in the uterus, or an ectopic pregnancy can be accurately assessed.
Diagnosis of ectopic pregnancy. A potentially life threatening condition when the pregnancy occurs in the wrong place, early diagnosis of ectopic pregnancy can be made through ultrasound and biochemical tests. Early diagnosis facilitates medical treatment and avoids a surgical operation. Thus appropriate medical or surgical treatment can be planned to avoid danger.
Diagnosis of multiple pregnancy and zygocity. Approximately 2% of women conceiving spontaneously and 10 -30% of women on fertility treatment will have a multiple pregnancy. At this stage of gestation it offers a unique opportunity to check if the fetuses share a common placenta, as this would have implications to for the rest of the pregnancy.
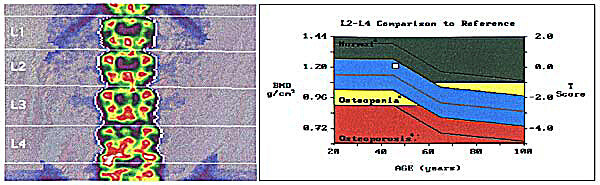
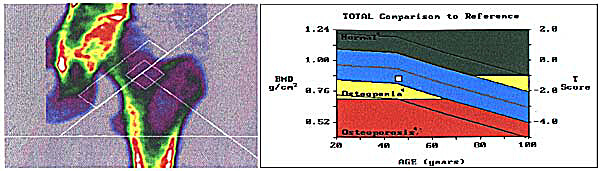
Screening for chromosomal abnormalities by nuchal translucency scanning between 11-14 weeks. By measuring the fluid behind the neck of the fetus at this stage of pregnancy, in combination with maternal age, we are able to give you a risk for major chromosomal abnormalities which is specific to you, You and your partner can then decide, based on the results, whether it’s high enough to warrant invasive prenatal diagnosis testing which can be chorionic villus sampling or amniocentesis later in the pregnancy.
Diagnosis of some major congenital abnormalities. Some of the major congenital abnormalities can be visualized at this early gestation, and allow for a plan of management to be decided upon.
Ultrasound Diagnosis in the Second Trimester
Fetal anomaly scan involving a detailed systematic survey of the fetus to detect congenital abnormalities and identify anatomical markers for chromosomal abnormalities. It is commonly done between the 18th to 22nd week of pregnancy. It allows major organs to be visualized and assessed as to its function and anatomy.
Doppler blood flow measurement : By measuring the blood flow in the uterine arteries at this stage of gestation, it is possible to pick out a sub-group of patients, which are at increased risk of developing pre-eclampsia and small babies. This allows treatment to commence at an early stage to modify the potential disease.
Placenta Location : A low-lying placenta, which covers the neck of the womb, may be a potential obstacle to a normal vaginal delivery. It may lead to serious bleeding later on in pregnancy endangering mother and baby. In cases where the placenta is visualized to be low at this gestation, we recommend that a scan should be repeated at 34th week, as most placental sites tend to move up and out of the way in late gestation as the uterus increases the size.
Diagnosis of Incompetent Cervix. By measuring the cervical length, it is possible to identify a group of patients who are at risk of premature labor, and it allows special management plan to be made for the pregnancy.
Ultrasound Diagnosis in the Third Trimester
Fetal Growth : The size and weight of the fetus can be determined by measuring a set of parameters. A scan is usually done around 32 - 33 weeks of gestation to screen for small gestational fetuses. Subsequent scans will be planned to monitor their growth.
Fetal Well-being : Ultrasound study of the behavior of the fetus constitutes the Biophysical Profile which is an indication of fetal well being. Together with Doppler Blood Flow we can find out if the fetus is happy and well inside the womb. It allows for an early detection of problems, and allows for treatment to minimize complications, including post delivery problems like cerebral palsy.
Identification of late fetal anomalies. Although relatively rare at this late stage to pick up any abnormalities in the fetus, it is possible that some fetal abnormalities might have been missed in early scans, or that certain conditions might have developed since the last scan.