What is IVF?
IVF is an effective form of assisted reproductive technology, one of the best bets for those with damaged or blocked tubes, unexplained sub-fertility, low sperm count or reduced sperm activity, severe endometriosis, or sub-fertility caused by antisperm antibody problems to become parents.
IVF means fertilisation outside the body. The fertilisation is done in a glass dish in the laboratory and the resulting embryo is replaced back into the womb.
Ovulation induction is usually carried out to increase the success rate by stimulating more follicles (eggs) and thereby increasing the chances of producing more embryos. Between one to two and at the most three embryos are normally transferred to optimise good pregnancy rates balancing against high order multiple births rate.
During the first initial consultation, semen analysis and blood tests will be performed. He should abstain for at least three days prior to the sample collection to have an accurate result. A sample can be submitted prior to the visit, and the result would be available during the consultation.
As part of the investigation for sub-fertility, all female patients are asked to have a baseline testing of three hormones, HIV, hepatitis and rubella status tested prior to the treatment. This, together with other investigation, would allow us to advise you on the best and most appropriate treatment for you.
Baseline hormone profiles need to be done on day 2 or 3 of the menstrual cycle. A luteal phase (2nd half of cycle) blood test to access for ovulation and progesterone may also be performed.
Once you have decided with the clinician which course of treatment you require, you have to sign the treatment consent forms. The treatment regime will be worked out and fully explained to you; your treatment may include the following procedures, namely ovarian stimulation, egg collection, fertilization and embryo transfer.
This will take place in two phases.
The treatment starts one week after ovulation. You may need ultrasound scans performed prior to treatment to ascertain the day of ovulation, and if all is normal, treatment will be started.
You may also be asked to commence on a combined contraceptive pill from day 5 of your normal cycle in order to prevent ovarian cyst formation which will lead to the commencement of the delay of treatment. In this case, treatment will start on the final 7 days of taking a packet of pills.
The aim of this phase is to achieve suppression of the brains natural stimulating hormones by using daily injections for 7 days. The ovary is under the control of the pituitary gland, which lies near the front of your brain. During you IVF cycle, the response from your ovaries may vary because of the influence of the pituitary gland. Suppression of the pituitary gland helps us to achieve optimum stimulation, increased number of eggs and embryos and most importantly prevent your ovary from releasing eggs prematurely at the wrong time prior to egg collection.
Potential side effects include hot flushes or night swears. Bleeding is normally noticed towards the end of the injection course.
You should call us on the first day you see your period so as to make an appointment to come in for a scan and blood test.
On day 2 or 3 of your period, you will have a scan performed to check that your ovaries look inactive and the lining of your womb (endometrium) is thin.
Once ovarian suppression is achieved, you will start daily injections of follicular stimulating hormone (FSH) to stimulate your ovaries to recruit a number of eggs.
Different drug regimes are used for stimulation. Your doctor will select the one most appropriate for you. The dosage of injection and the regime depend on your age, hormone levels, and previous response, if any.
You will have an ultrasound scan on day 5 or 6 of your stimulation to access the growth of follicles. The growth of follicles is monitored by ultrasound scanning. You will also be asked to provide to blood sample at 9am for the result to be ready at the time of consultation, which is required for adjusting the treatment according to the response.
You will be shown the response of your ovaries on the screen while you are having the ultrasound scan. You will usually be seen every other day for monitoring until you are ready for egg collection, which is usually on day 12 – 15 of the cycle.
When the patient is more advanced in age or has poor ovarian response from previous cycles, a shorter stimulation protocol will be used to improve the response rate. In this case, the stimulation will be started from day 2 / 3 of the cycle and add back suppression agent when the leading follicle reaches 12 – 14mm. This would prevent premature ovulation and the rest of the cycle proceeds in a similar fashion as above. This has an advent of a much shorter time required and is normally completed by three weeks after the onset of the period, as opposed to almost seven weeks with the long protocol.
When your follicles have reached an appropriate size (around 18mm), you will be ready for egg collection. You will be asked to have an injection of HCG (Human Chorionic Gonadotropin) and stop other injections. HCG mimics the natural process of LH release and triggers ovulation. It also helps in achieving the final ripening (maturity) of eggs and the timing of egg collection. Egg collection is normally planed around 36 hours after the HCG injection, and it must be done at an appropriate time.
On the day after HCG, you will have a ‘day off’ – you will not be having any injections or scan.
You will be asked to fast from midnight the night before prior to egg collection. Vaginal egg collection is performed under a short general anesthetic. A needle is passed through the vagina into the ovary where the follicles are present. The contents of the follicles are removed and examined under the microscope to see if an egg is present.
The procedure will take around 20 – 30 minutes, and it is not totally pain free. Discomfort may be experienced if you wake up from the anesthetic.
You are able to go home that afternoon when you recover from the effects of the anesthetic, and no excessive bleeding or pain is noticed. You are recommended to be accompanied by someone that evening. You may experience a dull ache or period like cramps in the lower part of your abdomen on the day of egg collection.
You will be told how many eggs were collected. You will be given some progesterone pessary to use to help maintain the lining of the womb for implantation. Antibiotics are also given to help you recover.
Your husband is asked to produce a semen sample by masturbation before you are taken into theatre for egg collection. This sample is assessed and if it is found suitable, it is washed in preparation and kept ready for fertilisation.
The semen sample provided by the male partner is washed and prepared. Progressively motile sperms are selected to inseminate the eggs. The eggs are normally inseminated between 40 – 42 hours after the HCG injection. We normally would do ICSI for all the viable eggs as this normally allows a greater chance of fertilisation.
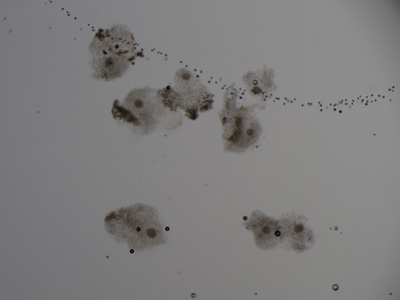
The eggs and the sperms are cultured overnight in an incubator. On the day after egg collection, the cultured eggs are examined microscopically to check for fertilisation.
Intra-Cytoplasmic Sperm Injection (ICSI). ICSI is for those whose sperm is of poor quality. With the ICSI procedure, a single sperm is injected in to the egg thus helping to fertilise it. Although this will increase the fertilisation rate, it also causes a small increase of congenital abnormality risk.
Assisted hatching will also be carried out for patients of more advanced age; sometimes the transparent zone of the egg can be too hard for the embryo to hatch out, which will lead to implantation failure. Assisted hatching is a procedure whereby the ‘hatching process’ is assisted in the laboratory by making a small hole in the shell of the embryo. This is achieved by using laser to thin out the shell of the embryo, allowing the embryo to be hatched out more easily.
To improve the quality of embryos, fragment removals may need to be done in certain cases.
Within 24 hours after fertilisation has occurred, the embryos will divide into two or four sells. The embryos are examined under the microscope for cell division and grading. Embryos are graded into four grades, with Grade 1 being the best. The transfer is normally done between day 2 and day 5 post egg collection, the exact timing will depend on the grade, the number of embryos, and how well they are dividing.
Embryo transfer procedure is performed by passing a fine tube through the neck of the womb (cervix). This is done under ultrasound scan control in order for the embryo to be placed in the optimal position. The embryos are injected high in the womb (uterus) in a minute amount of culture fluid. This technique does not normally require analgesia and is pain free. The procedure is quick, and you may leave after a few hours of rest.
After embryo transfer, you are advised to avoid intercourse and strenuous exercise post procedure. You will need to continue with the hormonal pessaries in order to help implantation of the embryos, and you may have to have injection of progesterone until the outcome of the treatment is out. One week after the egg collection, you will be asked to have a blood test performed, which determines if more supplements are needed. Some patients may need further injection of HCG.
14 days after the egg collection, you will be asked to perform a blood pregnancy test. If you test is positive, an ultrasound scan is performed 1 – 2 weeks later to check that the pregnancy is in the womb and also check the number of gestational sacs. Following this you will have an ultrasound scan two weeks later to confirm that the pregnancy is ongoing. You should be able to see the fetal heart at this stage.

The uterine cavity is the place where the embryo is to be implanted and the baby to grow. Should there be any abnormality in the uterine cavity, be it structurally or functionally, this can result in infertility or miscarriage.
Endometrial polyp
Endometrial polyp is an overgrowth of the inside lining of the uterus. Its presence will lead to distortion of the uterine cavity and make it unfavorable for the embryo to implant. It has been shown that removal of endometrial polyp in patients with infertility can improve pregnancy chance.
Uterine fibroid
Uterine fibroid is a very common benign gynaecological condition. Not all fibroids are related to infertility. It is mainly the submucosal fibroid (fibroid growing into uterine cavity) that will cause problems and worth surgical removal. Subserosal fibroid (fibroid growing over the outer surface of the uterus) usually does not require intervention. It is a controversial issue for the management of intramural fibroid (fibroid growing inside the muscular layer of the uterus). Surgical intervention might need to be considered for big size intramural fibroid (>4cm in diameter).
Adenomyosis
This is the condition when the inner endometrial lining of the uterus grows into its muscular layer. The uterus is diffusely enlarged and it is frequently associated with symptoms of significant period pain and heavy menstruation.
Intrauterine adhesion
Adhesion inside the uterine cavity is usually the result of surgical complication e.g. after uterine curettage or evacuation. Scarring, fibrosis and thinning of the uterine lining create an unfavorable environment for the embryo to implant and develop.
Congenital abnormality of the uterus
Septated uterus; double uterus are structural abnormalities related to miscarriage.
Diagnosis and Management:
Uterine abnormality may be first pick up by a screening ultrasound examination. Further evaluation is possible by infusing saline into the uterus during ultrasound assessment for a better delineation of the uterine cavity. Hysterosalpingogram can check both the uterine cavity and tubal patency.The gold standard for proper diagnosis of intrauterine abnormality will be by hysteroscopy. This is done by passing a small camera into the uterus through the cervix, via the vaginal route. Many corrective intervention can also be performed by hysteroscopic surgery.
Endometriosis is a condition when the tissue lining of the uterine cavity grows outside the uterus onto the peritoneum, ovaries and fallopian tubes. It is a progressive tissue and the condition has a high tendency to recur even after treatment. It commonly presents with menstrual pain or chronic pelvic pain. It is also frequently found during investigation for infertility.
The endometrial tissue outside the uterus responds to the menstrual cycle hormonal changes in the same way as the tissue lining the inside of the uterus. During menstruation, the blood that is to shed from the endometrial tissue in the abdominal cavity has no place to go, resulting in pooling of menstrual blood in the pelvic cavity and ovaries. This can lead to scarring of tissue, formation of adhesion, leading to blockage of fallopian tubes. Collection over the ovaries will result in the formation of chocolate cyst, leading to destruction of normal ovarian tissue and reduction in ovarian reserve.
For patients with endometriosis related tubal disease, In-Vitro Fertilization should be considered as treatment for infertility. Due to the impact of the disease itself or as a result of surgical excision of lesion, it is not infrequent the patient will have reduced ovarian reserve with poor egg quality and quantity. Early planning for pregnancy and resorting to assisted reproduction is advisable.
When an obstruction prevents the egg from traveling down the tube, the woman has a blocked fallopian tube. It can occur on one or both sides.
A tube may be obstructed due to infection such as pelvic inflammatory disease (PID). The Fallopian tubes may also be occluded or disabled by endometritis, infections after childbirth and intraabdominal infections including appendicitis and peritonitis. The formation of adhesions may not necessarily block a fallopian tube, but render it dysfunctional by distorting or separating it from the ovary.
Ovulatory dysfunction usually manifests as irregular, infrequent or absence of period. Anovulation is the condition when eggs are not properly developed from the ovary. There are various causes for anovulation. Investigations (including blood tests and imaging studies) should be carried out in order to establish the exact etiology of the condition so as to advise on the proper therapy for inducing ovulation.
For Hypogonadotrophic Anovulation (WHO Group I), the condition may be stress-induced or related to weight loss or excessive exercise. Occasionally, it may be due to organic pathology over the hypothalamic-pituitary axis. The treatment is mainly to correct the underlying cause, e.g. correction of weight and nutritional deficiency. Alternatively, ovulation induction can be achieved with gonadotrophins injections.
Majority of Normogonadotrophic Anovulation (WHO Group II) patients are suffering from polycystic ovarian syndrome (PCOS). PCOS patients may also suffer from other metabolic risk factors e.g. obesity, hyperandrogenism, diabetes, hypertension and atherosclerotic cardiovascular disease. For obese patients, weight reduction is useful in all aspects. Induction of ovulation can be very difficult and requires high level of experience and monitoring. The first line therapy is the use of anti-estrogens e.g. Letrozole. If this fails, second line therapies including that of metformin, laparoscopic ovarian drilling or gonadotrophins injection should be discussed and tailored to individual patient. Finally, for patients who have failed all these treatment options, In-Vitro Fertilization should be considered.
Hypergonadotrophic Anvoulation (WHO Group III) implies ovarian resistance or insufficiency / failure. Further investigations for the underlying cause will be required and the patient should start on hormonal replacement therapy. Options of oocyte donation, embryo donation or adoption should be considered.
For Hyperprolactinaemic Anovulation, further investigations will be required to exclude pituitary adenoma (by nuclear magnetic resonance imaging of pituitary gland) and hypothyroidism. Possibility of drug induced hyperprolactinaemia need to be explored. Treatment will be according to the cause. Dopamine agonist medications can normalize gonadal function. Patients with pituitary macroadenoma might require neurosurgical evaluation.
Male infertility can occur when there is a low sperm count, reduction in motility (movement) or normal morphology (appearance) of the sperms. In the majority of the conditions, no exact cause can be identified.
Sometimes, there might be history of genital infection, testicular trauma or exposure to radiation or certain medications which can lead to sperm production disorders. Occasionally, genetic defect is identified.
In all situations, quitting smoking, reducing alcohol intake and wearing loose fitting pants and underwear would be advisable.
For significant male factor, In-Vitro Fertilization (IVF) (and possibility of requiring Intracytoplasmic sperm injection – ICSI) would be the preferred mode of therapy. For mild male factor, intra-uterine insemination (IUI) may be considered, though there is recently controversial opinion on whether direct IVF is preferred to IUI in view of their individual success rate.
Sexual dysfunction or sexual malfunction is difficulty experienced by an individual or a couple during any stage of a normal sexual activity.
Sexual dysfunction takes different forms in men and women, it can also be life-long and always present, acquired, situational, or generalised, occurring despite the situation.
A man may be considered sexually dysfunctional if he does not ejaculate, experiences delayed ejaculation, is impotent, feels pain during intercourse. A woman’s sexual dysfunctions can be lack of or loss of sexual desire, has inadequate lubrication.
Many factors, of both physical and psychological natures, can affect sexual response and performance. Injuries, ailments, and drugs are among the physical influences. There is also an increasing amount of evidence that chemicals and other environmental pollutants depress sexual function. As for psychological factors, sexual dysfunction may have roots in traumatic events.
At the extreme end of Azoospermia (no sperms found in ejaculate), further investigation and referral to the Urologist to distinguish between obstructive Vs non-obstructive azoospermia will be required. Sophisticated assisted reproductive procedures using IVF with PESA/MESA/TESA (various methods of extracting sperms from the transporting tubules or from the testes) may be required. Alternatively, use of donor sperms may be another option.


While you are thinking about in vitro fertilisation (IVF) treatment, you may want to ask yourself the following few questions.
If you want to postpone giving birth because of your personal choice or your unfortunate circumstance such as cancer and severe endometriosis, it is possible to save your eggs or sperms for future use.
You may want to investigate other treatment options, such as IUI, before saying yes to IVF. Although IVF is not a high-risk treatment, it is the most complex of all fertility treatments and involves many different stages and hurdles.
The cost of IVF procedures can vary quite a lot so it’s a good idea to get an indication of costs up front.
The fees are usually split into several parts such as: consultation, diagnosis, screening, blood tests, drugs, operative procedures, embryo culturing and any other tests you may need.
It is not always a one-off payment, and you may be charged at different points for different procedures. So you need to make sure you are fully aware in advance of the total cost of all the steps involved in your case.
IVF may be demanding on you both physically and emotionally. Counselling services can be provided if you require.
The success rate of IVF varies from person to person. Success is dependent on a number of factors such as the woman’s age and the original reasons for the infertility. Generally speaking, the chances of a successful pregnancy drop as the age of the female increases beyond 35.
IVF, however, has significantly higher pregnancy rates than other treatments, and there may be extra embryos that can be frozen for subsequent pregnancy attempts, thus offering the potential for future pregnancies.
The risks of IVF are minor and we will discuss them with you before you begin the treatment, e.g. OHSS (ovarian hyperstimulation syndrome), operative risk. The most common health risk linked with IVF is multiple births (twins, triplets or more), therefore it is important for you to decide how many embryos to transfer in your treatment.
You can discuss these factors and any other concerns you may have by requesting a consultation session with us in which we will take you through the various procedures and recommend suitable treatments if needed.
IVF can help you overcome different causes of infertility and provide you with a better chance to have a baby, but it is not in itself the first step. The length of a complete treatment varies from couple to couple.
You can review the usual processes of the treatment below:
- 1.Pre-treatment consultation
- 2.Ovary preparation for egg production
- 3.Ultrasound and blood tests to determine the maturity of the eggs
- 4.Egg collection
- 5.Sperm preparation
- 6.Egg fertilisation
- 7.Embryo culture
- 8.Embryo transfer
- 9.Pregnancy test
At this point you just have to wait for nature to take over.
Before you make a decision about whether to proceed with fertility treatment, you must first have a consultation session with one of our fertility specialists to find out the causes of the infertility and if in vitro fertilisation is suitable for you.
Below are a few questions that people often ask before their first consultation visit:
You should bring original marriage certificate and all relevant records or laboratory results you may have and present them to our doctors.
This depends on your clinical condition. Our physician will discuss with you during the consultation session and arrange the appropriate investigation and treatment.
Usually within 2 weeks when you book with us.
The initial consultation normally lasts about 30 to 45 minutes.
You may be asked to do tests such as ultrasound examination, imaging studies, blood tests, or / and semen analysis.
Treatment periods vary. The duration of any IVF treatment depends on the kind of treatments required by each individual and the difficulties of the case.
Yes, as long as you wish.
Yes, you are always welcome if you wish to have a second opinion.
We prefer to see the couple together during the initial consultation. After appropriate investigation counselling, signing consent and when treatment starts, then the wife may come alone.